ATLANTA (AP) _ Getting an AIDS test at the drugstore could become as common as a flu shot or blood pressure check, if a new pilot program takes off.
The $1.2 million program will offer the free rapid HIV tests at pharmacies and in-store clinics in 24 cities and rural communities, the Centers for Disease Control and Prevention announced Tuesday.
“We believe we can reach more people by making testing more accessible and reduce the stigma associated with HIV,” Dr. Kevin Fenton, who oversees the agency’s HIV prevention programs, said in a statement.
The tests are already available at seven places, including Washington, D.C., Oakland, California, and an Indian health service clinic in Montana. The CDC will soon pick 17 more locations.
The HIV test is a swab inside the mouth; it takes about 20 minutes for a preliminary result. The test maker says it’s correct 99 percent of the time. If the test is positive for the AIDS virus, pharmacy employees will refer customers to a local health department or other health care providers for a lab blood test to confirm the results, counseling and treatment. The workers are expected to deliver the news face-to-face and give customers privacy, the CDC said.
An estimated 1.1 million Americans are infected with HIV, but as many as 20 percent of them don’t know they carry the virus, according to the CDC. It can take a decade or more for an infection to cause symptoms and illness.
Since 2006, the CDC has recommended that all Americans ages 13 to 64 get tested at least once, not just those considered at highest risk: gay men and intravenous drug users. But fewer than half of adults younger than 65 have been tested, according to the agency’s most recent statistics.
It’s important to know about infection not only for treating the condition but also to take steps to prevent spreading it to others. An HIV diagnosis used to be a death sentence, but medications now allow those infected to live longer and healthier lives.
On special occasions, health organizations have sent workers to some drugstores to offer HIV testing. This week, Walgreens, the nation’s largest chain of pharmacies, is teaming with health departments and AIDS groups to offer free tests in 20 cities.
But in that program, health professionals conduct the tests and deliver the news. The CDC program aims to train pharmacy staff to test and deliver the results themselves.
“I’m excited. It’s such a new and novel thing for us,” said Sarah Freedman, who manages a Walgreens in Washington, D.C., that is participating in the pilot program.
At her pharmacy, prominent signs advertise the test, which is then done in a private room. The pharmacy has also taken steps to let a customer discreetly request the test, putting out stacks of special test request cards (they look like business cards) at George Washington University and nearby businesses. Anyone seeking a test can simply hand the card to the clerk, she said.
Only three or four customers have gone through with a test in the first few weeks.
“We get a lot of questions,” she said. “Usually they get the information and they go and sit on it and think about it.”
The drugstores are expected to keep the test confidential. Pharmacy workers are to refer customers with positive tests to counseling and other services.
When the project ends next summer, CDC officials will analyze what worked well and what didn’t, said Paul Weidle, the epidemiologist who is heading up the project.
The program carries both promise and potential pitfalls, said Julie Davids, a longtime advocate who now works for the AIDS Foundation of Chicago.
More testing is a plus, she said. And even if they don’t get a free test, signs in the drugstores may prompt people to get tested at a doctor’s office or clinic where they feel more comfortable, said Davids.
But Davids said pharmacies more used to handling cholesterol screenings might have difficulty responding to patients who learn in a drugstore they’re HIV-positive.
“A person may freeze up and fall apart later,” or get emotional on the spot and even talk about suicide, she said.
In addition to Freedman’s store, a second Walgreens in Washington is offering the test, as well as branches in Chicago and Lithonia, Georgia. The other sites are East Pines Pharmacy in Riverdale, Maryland, Mike’s Pharmacy in Oakland, California and a federal Indian Health Service location in Billings, Montana.
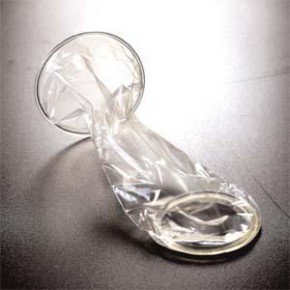
Each location will get enough tests to check 200 to 300 people. Made by OraSure Technologies Inc., the $17.50 test is the only government-approved rapid HIV test that uses saliva. Other rapid tests on the market analyze a finger-prick blood sample. The tests are used routinely in doctor’s offices, hospitals and clinics.
The OraSure swab test’s stick-like testing device is used to wipe the inside of the mouth, then it is put in a solution, said company spokesman Ron Ticho. If two lines appear, that indicates a positive test.
The company is seeking government approval to sell it over-the-counter for home testing. A decision is expected later this year.
The test is sold in about 40 countries, including Mexico, Italy, South Korea and South Africa. Ticho said he is not aware of another country where pharmacies routinely offer the testing.
 From lehighvalleylive.com…
From lehighvalleylive.com…
 This month, the Centers for Disease Control and Prevention expanded the national HIV awareness and anti-stigma campaign,
This month, the Centers for Disease Control and Prevention expanded the national HIV awareness and anti-stigma campaign, 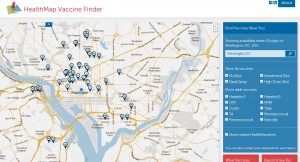

 Health regulators on Tuesday said they approved OraSure Technologies Inc’s in-home test for HIV, making it the first over-the-counter, self-administered test for the virus that causes AIDS.
Health regulators on Tuesday said they approved OraSure Technologies Inc’s in-home test for HIV, making it the first over-the-counter, self-administered test for the virus that causes AIDS.![can_front_png[1]](https://m4mhealthinfo.org/wp-content/uploads/2012/07/can_front_png1.png?w=242&h=171)
