From The Morning Call, October 09, 2010|By Jarrett Renshaw
20% of gay men have HIV and nearly half don’t know they’re infected
Men who have sex with men (MSM) still make up the largest percentage of new HIV infections in the U.S. Despite the grass-roots effort to educate gay and bi men since the 1980’s, the number of new infections continues to rise. A recent study conducted by the Centers for Disease Control and Prevention makes the issue clear.
From the Centers for Disease Control and Prevention (CDC) Website…
The CDC estimates that more than one million people are living with HIV in the United States. One in five (or 21%) don’t know they’re infected. Despite increases in the total number of people living with HIV in recent years, the annual number of new HIV infections has remained relatively stable. However, that still means an estimated 56,300 new infections per year.
More than 18,000 people with AIDS still die each year in the US. Gay, bisexual, and other MSM are strongly affected and represent the majority of persons who have died. Gay, bisexual, and other MSM of all races remain the population most severely affected by HIV. Here are some facts you need to know:
- MSM account for more than half (53%) of all new HIV infections in the U.S. each year, as well as nearly half (48%) of people living with HIV.
- While CDC estimates that MSM account for just 4% of the US male population aged 13 and older, the rate of new HIV diagnoses among MSM in the US is more than 44 times that of other men and more than 40 times that of women.
- White MSM account for the largest number of annual new HIV infections of any group in the US, followed closely by black MSM.
- MSM is the only risk group in the U.S. in which new HIV infections have been increasing since the early 1990s.
What can you do?
The first thing you can do is get tested. Second, practice safer sex. I know we’re all tired of hearing this but clearly the message still needs to be broadcast loud and clear. There are any number of online resources that will help you to play safe and stay healthy. Just using a condom is only a small part of what you need to know. In addition to our own HIV Education page, you can go to any one of these links to educate yourself and to protect your health:
About.com’s page for gay teens
To check out the CDC’s full report, you can go to the CDC’s Website.
To subsribe to the Pitt Men’s Study Health Alerts, send an email to rgy2@pitt.edu with the word subscribe in the subject line.
Speaking of lubes, UCLA researchers found 4 out of 6 most used lubes are toxic to rectal lining
This bit of information was pointed out by a Facebook subscriber in Texas. One of the studies mentioned in the article is actually right here at the University of Pittsburgh – The Microbicides Trials Network. You can find out more about it under our “Get Involved in Research” tab.
As the article notes: “Subjects who used lubricants during anal sex were three times more likely to contract rectal sexually transmitted infections than those who had anal sex without lubricant, found UCLA researchers. This and one other study examining the effects of sexual lubricants used in anal sex were presented last month at the International Microbicides Conference.” The bottom line is two of the lubes tested were found to be nontoxic – Wet Platinum and PRÉ.
To read the full article, go to 365gay.
Health Alert – N9
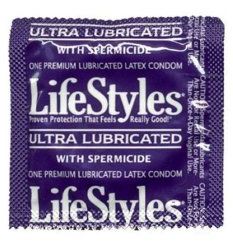 Nonoxynol-9 (or N-9) was created in the 1980’s as a spermicide—a method of contraception. The substance was also thought to prevent sexually transmitted diseases and it even killed HIV (the virus that causes AIDS) in test-tube studies. As a result, many gay and bisexual men who engaged in anal sex adopted the use of condoms and lubricants containing N-9 as a means to prevent HIV. Increased Risk for HIV Infection More recently, however, researchers have discovered N-9 can damage the lining cells of the rectum during anal sex, making a person more susceptible to contracting HIV.
Nonoxynol-9 (or N-9) was created in the 1980’s as a spermicide—a method of contraception. The substance was also thought to prevent sexually transmitted diseases and it even killed HIV (the virus that causes AIDS) in test-tube studies. As a result, many gay and bisexual men who engaged in anal sex adopted the use of condoms and lubricants containing N-9 as a means to prevent HIV. Increased Risk for HIV Infection More recently, however, researchers have discovered N-9 can damage the lining cells of the rectum during anal sex, making a person more susceptible to contracting HIV.
What’s so troubling is that men who have sex with men are either unaware of this danger or don’t believe the danger actually exists. In fact, a study performed in San Francisco found that one quarter of respondents reported using lubricants containing N-9 despite repeated warnings from the Centers for Disease Control and Prevention, the World Health Organization and the Gay and Lesbian Medical Association to not use N-9 when engaging in anal intercourse. What Can You Do? Don’t use lubricants, condoms, or any other product that contains N-9. If the package says “spermicidal lubricant” on the box avoid it! The best way to prevent HIV infection when engaging in anal intercourse is to use latex condoms and water-based lubricants. To learn more about N-9, you can go to this informative page on About.com.
Top ten health issues for men who have sex with men
1. HIV/AIDS, Safer Sex
That men who have sex with men are at an increased risk of HIV infection is well known, but the effectiveness of safe sex in reducing the rate of HIV infection is one of the gay community’s great success stories. However, the last few years have seen the return of many unsafe sex practices. While effective HIV treatments may be on the horizon, there is no substitute for preventing infection. Safe sex is proven to reduce the risk of receiving or transmitting HIV. All health care professionals should be aware of how to counsel and support maintenance of safe sex practices.
2. Substance Use
Gay men use substances at a higher rate than the general population, and not just in larger communities such as New York, San Francisco, and Los Angeles. These include a number of substances ranging from amyl nitrate (“poppers”), to marijuana, Ecstasy, and amphetamines. The long-term effects of many of these substances are unknown; however current wisdom suggests potentially serious consequences as we age.
3. Depression/Anxiety
Depression and anxiety appear to affect gay men at a higher rate than in the general population. The likelihood of depression or anxiety may be greater, and the problem may be more severe for those men who remain in the closet or who do not have adequate social supports. Adolescents and young adults may be at particularly high risk of suicide because of these concerns. Culturally sensitive mental health services targeted specifically at gay men may be more effective in the prevention, early detection, and treatment of these conditions.
4. Hepatitis Immunization
Men who have sex with men are at an increased risk of sexually transmitted infection with the viruses that cause the serious condition of the liver known as hepatitis. These infections can be potentially fatal, and can lead to very serious long-term issues such as cirrhosis and liver cancer. Fortunately, immunizations are available to prevent two of the three most serious viruses. Universal immunization for Hepatitis A Virus and Hepatitis B Virus is recommended for all men who have sex with men. Safe sex is effective at reducing the risk of viral hepatitis, and is currently the only means of prevention for the very serious Hepatitis C Virus.
5. STDs
Sexually transmitted diseases (STDs) occur in sexually active gay men at a high rate. This includes STD infections for which effective treatment is available (syphilis, gonorrhea, chlamydia, pubic lice, and others), and for which no cure is available (HIV, Hepatitis A, B, or C virus, Human Papilloma Virus, etc.). There is absolutely no doubt that safe sex reduces the risk of sexually transmitted diseases, and prevention of these infections through safe sex is key.
6. Prostate, Testicular, and Colon Cancer
Gay men mar y be at risk for death by prostate, testicular, or colon cancer. Screening for these cancers occurs at different times across the life cycle, and access to screening services may be negatively impacted because of issues and challenges in receiving culturally sensitive care for gay men. All gay men should undergo these screenings routinely as recommended for the general population.
7. Alcohol
Although more recent studies have improved our understanding of alcohol use in the gay community, it is still thought that gay men have higher rates of alcohol dependence and abuse than straight men. One drink daily may not adversely affect health, however alcohol-related illnesses can occur with low levels of consumption. Culturally sensitive services targeted to gay men are important in successful prevention and treatment programs.
8. Tobacco
Recent studies seem to support the notion that gay men use tobacco at much higher rates than straight men, reaching nearly 50 percent in several studies. Tobacco-related health problems include lung disease and lung cancer, heart disease, high blood pressure, and a whole host of other serious problems. All gay men should be screened for and offered culturally sensitive prevention and cessation programs for tobacco use.
9. Fitness (Diet and Exercise)
Problems with body image are more common among gay men than their straight counterparts, and gay men are much more likely to experience an eating disorder such as bulimia or anorexia nervosa. While regular exercise is very good for cardiovascular health and in other areas, too much of a good thing can be harmful. The use of substances such as anabolic steroids and certain supplements can adversely affect health. At the opposite end of the spectrum, overweight and obesity are problems that also affect a large subset of the gay community. This can cause a number of health problems, including diabetes, high blood pressure, and heart disease.
10. Anal Papilloma
Of all the sexually transmitted infections gay men are at risk for, human papilloma virus —which cause anal and genital warts — is often thought to be little more than an unsightly inconvenience. However, these infections may play a role in the increased rates of anal cancers in gay men. Some health professionals now recommend routine screening with anal Pap Smears, similar to the test done for women to detect early cancers. Safe sex should be emphasized. Treatments for HPV do exist, but recurrences of the warts are very common, and the rate at which the infection can be spread between partners is very high.
From the Gay Lesbian Medical Association Website.
Author: Vincent M. B. Silenzio, MD, MPH, Former Member Board of Directors, GLMA and Former Co-Editor, Journal of the Gay and Lesbian Medical Association
Health Alert – Testicular Cancer
Testicular cancer is the most common cancer in men between 20 and 34 years old. It is a disease in which cancer forms in one or both testicles. The testicles are 2 egg-shaped glands inside the scrotum (a sac of loose skin that lies directly below the penis). They are the male sex glands that make testosterone and sperm.
Risk Factors
There are factors that raise a man’s risk of getting this disease:
- An undescended testicle – One or both testicles don’t move from the abdomen into the scrotum during fetal development.
- Certain types of moles – An unusual condition that causes many spots or moles on the back, chest, abdomen and face.
- HIV Infection – Men infected with HIV have an increased risk, especially true for men who have AIDS.
- Carcinoma in situ (CIS) – CIS is a condition in which germ cells grow into a tumor but does not yet invade normal tissues. CIS in the testicles may become cancer over a number of years and does not cause a lump or any symptoms.
- Young age – Young men have a higher risk of getting testicular cancer. It is the most common cancer between the ages of 20 to 34, the second most common cancer between the ages of 35 to 39, and the third most common cancer between the ages of 15 to 19.
- A personal history of testicular cancer – Men who already had testicular cancer have a higher risk of developing a tumor in the other testicle.
- A family history of testicular cancer – Men with a family history of testicular cancer may have a higher risk of developing testicular cancer.
- Congenital abnormalities – Men born with abnormalities of the testicles, penis, or kidney, as well as those with a hernia in the groin area, where the thigh meets the abdomen, may be at increased risk.
Signs
Possible signs of testicular cancer include:
- a painless lump or swelling in either testicle
- heaviness or aching in the abdomen or scrotum
- pain or discomfort in a testicle or in the scrotum
- dull ache in the lower back, abdomen, or groin
Treatment
If testicular cancer is found, the treatment depends on the stage of the cancer. Three standard treatments are used:
- Surgery. Surgery removes the testicle and some of the lymph nodes (organs that fight infection). Tumors that have spread to other places in the body may be partly or entirely removed by surgery.
- Radiation therapy. High-energy x-rays or other types of radiation kill cancer cells.
- Chemotherapy. Drugs are used to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing.
Self Exam
Most men find the cancer in their testicles themselves. This fast and simple exam can help you find this cancer early. Do the exam after a warm bath or shower every month. Also ask your health care provider to do a testicular exam as part of your regular checkup.
The Testicular Cancer Resource Center provides information about how to do a testicular cancer self examination. Go to http://tcrc.acor.org/tcexam.html for more information.
For more information, go to…
National Cancer Institute: http://www.cancer.gov/cancertopics/factsheet/sites-types/testicular
New National Plan to Fight HIV
President Obama unveiled his domestic HIV/AIDS plan – a $30-million initiative that focuses significantly on prevention efforts among men who have sex with men. Read more from the Philadelphia Gay News.
HIV [is still a] Big Deal
“The core component of the HIV Big Deal project is a series of 10-minute video dramas that realistically address the social and health-related dilemmas gay men face. So far, two episodes have been released, and more are in production.”
If you haven’t watched the videos, you should. In fact, they should be required viewing for any guy who has sex with other guys. If you’re HIV positive, HIV Big Deal also wants to hear from you. Share your stories about disclosing your HIV status for their new video production, Ask Me, Tell Me.
A Word Form Your Local “Online Sexual Health Educator”
By: Ray Yeo
It’s been a little over a year since the Pitt Men’s Study started reaching out to guys in places like craigslist, gay.com and adam4adam. For the most part, I’d say we’ve been successful in getting our foot in the door and letting folks know we’re online to provide much-needed information about sexual health. But, as with many health intervention programs, there’s a core group of folks that still aren’t getting the message about avoiding sexually transmitted infections, including HIV.
We know that new HIV infections are still on the rise in Pennsylvania—even after all the grass roots sex education that happened early on, when the epidemic first laid waste to the gay community. There’s been a lot of talk about why the virus is still spreading and lots of folks agree we need to step up or efforts to continually educate the public about the risks of unsafe sex. But the one thing I don’t see a lot in the mainstream media is how finding sexual partners on the Internet plays a significant role in these new infections.
Mounting research indicates that guys who hook up online for sex (as apposed to traditional venues like bars and bath houses) have sex more often, have unprotected sex more often, and have more sex with guys who are HIV-positive. So it would seem pretty clear that we need to get our safer sex messages into the same chat rooms where these folks are hooking up.
One of our challenges is that, like the bars and bath houses in the early 1980’s, the owners of sex-related Websites don’t necessarily want to bring up issues of sexual health for fear that it will put off their clientele. The person in charge at Manhunt told me once that if their guys feel harassed by a sexual health educator, they’ll just take their business to gay.com. As a result, on Manhunt, I can’t advise guys about sexual health unless they chat with me first. The problem then, of course, is that if a person is online just for sex, he’s probably not going to make contact with me. The other problem is that guys often don’t know they’re at risk and, therefore, don’t know to ask for safer sex information. So how do we get the word out to guys who are living in an online bubble that’s devoid of safer sex messages?
One solution is to spread the word that men who are looking for sex with men on-line do need special sexual health information. We all know we’re supposed to use a condom for anal sex, but how many guys know that drinking and using drugs can lower your inhibition and turn a moment of safe sexual pleasure into (at best) prolonged medical treatments? How many guys know that, if you don’t like to use a traditional condom (for anal sex) because it doesn’t feel good, you can use a female condom instead? Would you know to call your doctor and ask for immediate “post-exposure prophylaxis” treatment if you know you’ve been exposed to HIV in the last 72 hours?
Another potential solution is to expand our online presence. To this end, we’ve created the gay/bi friendly Website m4mHEALTHYsex.org—a place where guys can go to find out about HIV and other STDs. The site hosts user-friendly “sexual health avatars”—animated characters who can answer basic questions about sexually transmitted diseases. Users can also search by zip code to find information like gay-friendly medical providers and local testing centers. And, if for some reason a person can’t find the information he’s looking for, the user can email the staff at the Pitt Men’s Study and pose questions to our staff of medical professionals (folks who’ve been dealing with the health of gay and bi men for 25 years).
We’ve come a long way in the treatment for HIV infection. And although modern anti-viral drugs are a genuine life-saving breakthrough, we still don’t have a cure or a vaccine to prevent it. Furthermore, as anyone on those miraculous antiviral drugs will tell you, having HIV is still a life-altering experience—and not in a good way.
In short, getting the gay and bi male community to understand that they still need information about safer sex is critical. If you’re picking up guys online for sex, you may be treading on thin ice. You may think you know it all, but, as the indisputable numbers of new HIV infections becomes more apparent, you might want to think twice when you see that “online sexual health educator” profile on Manhunt. Go ahead, ask me a question. I might be able to put you on the right track toward a better, safer sex life.
FDA approves more advanced HIV test
WASHINGTON, June 21 (Reuters) – The U.S. Food and Drug Administration has approved a test that may help slow the spread of HIV by detecting the virus more quickly in the early period when it is most infectious…
Read the full story on Reuters.
Gay-Friendly Health Network
Health Network changes Patients’ Bill of Rights to fully protect LGBT patients and their families from discrimination at 430 medical offices and 36 hospitals. Read about Kaiser Permanente on PinkPaper.com.
“We need to re-ring the alarm about HIV transmission among gay and bisexual men.”
“After miracle breakthroughs in treatment and two decades worth of increasingly sophisticated understanding about sexually transmitted diseases, how did we end up back at the beginning with gay and bisexual men so vulnerable to infection?”
Find out the answer on the Boston Globe Website, boston.com
Syphilis Outbreak – originally posted in April of 2008
 Officials at the Centers for Disease Control and Prevention (CDC) recently reported that syphilis rates continued to rise in 2007. The disturbing fact is that the surge is being driven by cases among men who have sex with men (MSM), who accounted for 64 percent of the known syphilis infections last year. That’s up from five percent in 1999. It is important to note that Symptoms of syphilis can go unnoticed or misdiagnosed. The CDC’s website notes: “Many people infected with syphilis do not have any symptoms for years, yet remain at risk for late complications if they are not treated. […] Thus, transmission may occur from persons who are unaware of their infection.”
Officials at the Centers for Disease Control and Prevention (CDC) recently reported that syphilis rates continued to rise in 2007. The disturbing fact is that the surge is being driven by cases among men who have sex with men (MSM), who accounted for 64 percent of the known syphilis infections last year. That’s up from five percent in 1999. It is important to note that Symptoms of syphilis can go unnoticed or misdiagnosed. The CDC’s website notes: “Many people infected with syphilis do not have any symptoms for years, yet remain at risk for late complications if they are not treated. […] Thus, transmission may occur from persons who are unaware of their infection.”
What is the danger?
Syphilis is especially worrisome because, if it goes untreated, it can lead to serious health conditions later on in life. It can also complicate other infections such as HIV. It is also important to note that Syphilis can be transmitted through a variety of sexual acts, not just intercourse. So a condom won’t necessarily protect you.
Signs of Syphilis
Syphilis usually begins with the appearance of a single sore (called a chancre), but there may be multiple sores. The time between infection with syphilis and the start of the first symptom can range from 10 to 90 days. The chancre is usually firm, round, small, and painless. The chancre lasts 3 to 6 weeks, and it heals on its own. Note, however, that the infection doesn’t’ go away without proper treatment.
As the disease progresses, it may include fever, swollen lymph glands, rash, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and fatigue. The signs of this “secondary stage” of syphilis will resolve with or without treatment, but, again, it doesn’t go away.
In its later stages, many years after the initial infection, the disease can cause damage to internal organs, the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. Signs and symptoms of the “late stage” include difficulty coordinating muscle movements, paralysis, numbness, gradual blindness, and dementia. This damage may be serious enough to cause death.
What can you do?
Get tested. All sexually active MSM should receive testing for a wide range of sexually transmitted diseases at least once a year (as recommended by the CDC).
You’re not going to hear much about this in the mainstream media and, chances are, your doctor isn’t going to recommend being tested for an STD. So it’s up to you to take matters into your own hands. Syphilis is easily cured in its early stages. A single injection of penicillin will cure a person who has had syphilis for less than a year. Additional doses are needed to treat someone who has had syphilis for longer than a year. For people who are allergic to penicillin, other antibiotics are available.
Your doctor can perform the test for syphilis. The Allegheny County Health Department also provides free testing. You can find other local testing sites (some will maintain your anonymity) at http://www.stopHIV.com in the drop-down resources menu, under “PA Service Providers.”
For more information about MSM and syphilis, you can go to the CDC’s Syphilis and MSM web page
Rights of People With HIV Under Assault?
 Although a recent New York Times article (posted below) suggests immediate treatment for HIV-positive men has a long-term beneficial effect on health, activist Sean Strub argues the policy focuses too much on prevention and not on the needs of persons living with the disease. His editorial, Medical Ethics and the Rights of People With HIV Under Assault was posted on POZ blogs on April 28th.
Although a recent New York Times article (posted below) suggests immediate treatment for HIV-positive men has a long-term beneficial effect on health, activist Sean Strub argues the policy focuses too much on prevention and not on the needs of persons living with the disease. His editorial, Medical Ethics and the Rights of People With HIV Under Assault was posted on POZ blogs on April 28th.
HPV and Men – originally posted January 2008
What is HPV?
Human papillomavirus (HPV) is a sexually transmitted disease that infects the genital area of both men and women (including the skin on and around the anus). Over half of the men in the United States will have HPV at some time in their lives. Often the virus clears up on its own without a health problem but, depending on the strain of HPV, it can cause genital or anal warts. Some strains of HPV can also cause abnormal changes in cells which can become precancerous and result in cancer of the penis or anus. HIV positive men are more likely to get severe and prolonged cases of genital warts which may be resistant to treatment.
How is HPV spread?
HPV is passed through vaginal or anal intercourse but can also be spread through simple skin to skin contact. Because HPV infections often don’t have symptoms, they can be passed on unknowingly.
What are the symptoms?
Genital warts are the first symptoms seen with low-risk strains of HPV infections. They are soft, raised growths that are usually painless. These lesions can also appear in the mouth and throat, although this is rare. Warts usually take 3 weeks to 6 months to appear after exposure but, in some cases, can also take years.
What can I do?
If you are diagnosed with HPV, it is important to tell your sexual partner(s). Transmission of HPV can be minimized by finding alternative ways to express intimacy and avoiding contact with a wart. Condoms are also effective for preventing infection with HPV if they are used correctly and consistently. However, genital warts not covered by a condom can still transmit the virus
14 percent of gay men in DC are HIV positive
DC Department of Health: 14 percent of gay men in DC are HIV positive–that’s almost five times as high as the overall rate. A quote from their study reads “complacency that the HIV/AIDS epidemic is under control for men who have sex with men has taken a toll.”
It’s pretty convincing evidence that HIV is still very much with us. The pdf link to the official report takes an extra minute to open.
Pitt Men’s Study Director Creates Anal Dysplasia Clinic
Dr. Ross Cranston was recruited to Pittsburgh in 2007 to create an Anal Dysplasia Clinic at the Pittsburgh AIDS Center for Treatment (PACT). The focus of the clinic, which is also open to non-PACT patients, is to address the high incidence of human papillomavirus (HPV or wart virus). HPV has been associated with anal cancer in gay men – particularly those living with HIV.
“As gay men, we run the risk of serious health issues because we don’t pay enough attention to our butts.” Dr. Cranston states. “So, one of my goals is to promote an ‘anal agenda’ that increases awareness of the medical conditions gay men are more likely to experience.” Putting the issue into perspective, he adds: “Anal health has yet to emerge as an area to which it is deemed appropriate to direct our attention. As a result, gay men in particular are unaware of their increased risk of many anal diagnoses including those related to sex or sexually transmitted infections, such as the development of anal cancer.”
Patients with an abnormal anal cytology (a test of anal cells that is used to detect abnormalities) are referred to Dr. Cranston for high-resolution anoscopy (HRA). This office procedure involves examining the anal canal using magnification. If there is evidence of high-grade dysplasia – the precursor to anal cancer – a biopsy may be performed. If high-grade dysplasia is confirmed, Dr. Cranston can then remove the lesion in order to prevent its potential progression to cancer.
“We are currently diagnosing about one case of anal cancer every 2 weeks,” says Dr. Cranston, “which is why I suggest that gay men who are HIV-positive talk to their clinician about anal dysplasia screening and have an annual anal Pap smear.” Although there are no national screening guidelines, Dr. Cranston notes, it is also suggested that HIV-negative men over 40 get tested every two to three years.
Dr. Cranston is an Assistant Professor in the Division of Infectious Disease and the Medical Director of the Pitt Men’s Study. He began his studies at the University of Edinburgh before moving to London, where he completed a fellowship in HIV and Sexually Transmitted Infection. He moved to the U.S. to conduct doctoral research at the University of California—San Francisco and then spent five years working at the UCLA Center for AIDS Research and Education in Los Angeles, where he established and ran the UCLA Anal Dysplasia Clinic.
For many years, Dr. Cranston has used his knowledge of anal dysplasia, HPV, and HIV to help countless HIV-positive men. He moved to Pittsburgh in September 2007 with his partner of 11 years, Ian McGowan, who is also employed by the University as a Professor in the School of Medicine, and is Co-Principal Investigator of the Pittsburgh-based Microbicide Trials Network.
For more information about the anal dysplasia clinic, you can call 412-647-0996 .
female condom for anal sex
You can use a female condom as an alternative to the traditional male condom for anal sex. Here’s how… (click on the image below).
Testing Microbicides to Combat HIV
The development of safe and effective prevention strategies against HIV infection is a critical component of the HIV research agenda and, in recent years, the University of Pittsburgh School of Medicine has emerged as a global leader in microbicide development. Ongoing microbicide research is based both in Pittsburgh and at international sites in Africa and India.
A microbicide is a substance designed to prevent transmission of HIV and other sexually transmitted diseases in men and women. It can come in the form of a gel, cream, suppository, film, sponge or ring that releases an active ingredient over time.
The Microbicide Trials Network (MTN) is led by Dr. Sharon Hillier and headquartered at Magee-Womens Research Institute & Foundation in Pittsburgh. The MTN is funded by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health specifically to conduct clinical trials to evaluate the safety and effectiveness of topical microbicides. Several microbicides are being tested in clinical trials and the present network includes a total of 17 sites located in seven countries.
The concept for a microbicide-like product was developed more than 15 years ago by reproductive health specialists and advocates who recognized the need for female-controlled HIV prevention methods. Beyond being effective, microbicides for HIV prevention must be safe and easy to use.
Microbicides first undergo rigorous testing in the laboratory before testing in humans can occur. Phase I trials evaluate safety in a small number of people exposed to study products for brief periods such as one to two weeks. If those study results suggest the product is safe, investigation then progresses to a Phase II trial. Researchers then track safety of the product over greater periods of time.
Finally, Phase III trials are performed to establish the product’s effectiveness. This type of study is conducted in a large number of participants, and usually involves multiple centers. Studies may be designed to compare one product’s effectiveness with another’s and/or with an inactive agent, or placebo. The data resulting from a Phase III trial are often used by regulatory agencies to determine if a product should be approved for widespread use.
Public health experts estimate microbicides that are even 60 percent effective against HIV could prevent upwards of 2.5 million infections over a three-year period. More research is focusing on the development of rectal microbicides. One current trial involves assessment of rectal safety of microbicide products originally formulated for the vagina, as it is assumed that once vaginal microbicides are licensed they will also be used in the rectum. In addition, a team lead by Dr. Ian McGowan are developing microbicide products formulated specifically for rectal use.
For information about microbicides, the following websites offer a variety of views and news including research and advocacy efforts. They are: http://www.mtnstopshiv.org/; http://www.ipm-microbicides.org/; http://www.global-campaign.org/; and http://www.microbicide.org/.
Persons interested in participating in upcoming local microbicide research studies at the University of Pittsburgh are encouraged to call Anne Davis at 412-641-3381 .
Health Department Tests Online Partner Notification
The Allegheny County Health Department has begun testing an online partner notification system. The online system is designed to send anonymous “e-card” messages to persons who may have been exposed to a sexually transmitted disease. “The way it works,” explains Raymond Yeo, a University of Pittsburgh consultant involved in creating the system, “is that if I were to test positive for Syphilis or HIV, for example, I would go online with a Department of Health representative and send email messages to all the people I’ve had sex with.” Yeo works for Pitt’s Graduate School of Public Health as an online sexual health educator. “The internet has become a major venue for finding sexual partners,” Yeo went on to explain, “so the Pennsylvania Department of Health needed to create a method of contacting people who may have been exposed to sexually transmitted diseases when the only contact information they have is an email address.”
The e-card message informs recipients that a person they’ve hooked up with (for sex) tested positive for an undisclosed sexually transmitted disease and encourages him or her to also get tested. Messages also contain a unique identification number that medical providers and clinics can use to determine what infection they should test for. This number is also reported back to the Department of Health for the purpose of tracking state-wide outbreaks.
“If you receive an e-card from the Pennsylvania Department of Health, telling you that you’ve been exposed to a sexually transmitted disease, you can take it seriously because the system is controlled by the Health Department staff…which pretty much eliminates the possibility of it being a hoax or a spam message,” Yeo added. “It’s important that this system succeeds in what it was designed to do. Folks who are hooking up on the Internet for sex are getting infected at higher rates than folks who don’t…and if we don’t find a way to contact them, and they don’t get tested, it will only lead to bigger health problems for our community.”
People who have been exposed to a sexually transmitted disease, in cases where additional contact information is available (such as a phone number or mailing address), are contacted via traditional methods. For more information about the Pennsylvania Health Department Online Notification System, you can contact Mr. Yeo at the University of Pittsburgh’s Graduate School of Public Health by calling (412) 383-2940 . You can also go to the Partner Notification Website at http://www.pastatehealth.org/.



